Fact vs. Fiction: Topical Steroid Withdrawal
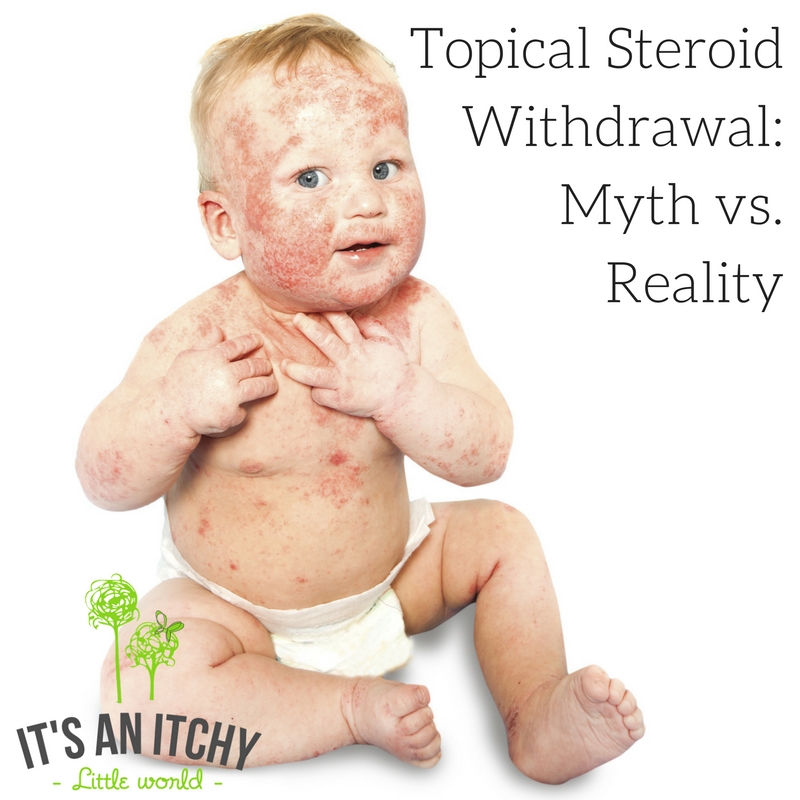
Topical Steroid Withdrawal exists, but thankfully it isn’t as widespread as you may think. Read on to learn more.
By Neil R. Lim, BA and Peter A. Lio MD (see bio below)
Topical corticosteroids (TCS) were hailed as a modern medical miracle when they made their debut over 60 years ago. For the first time, many inflammatory diseases that caused a tremendous amount of suffering could be quieted. While certainly not a silver bullet and clearly not without side effects, TCS represent the mainstay of treatment for eczema and are universally recognized as a safe and effective therapy when used properly (Hajar). Nevertheless, a rapidly-growing fear among patients and parents of patients afflicted with atopic dermatitis is that of topical steroid “addiction” and subsequent symptoms of topical steroid “withdrawal” after stopping the medication also called Red Skin Syndrome in some circles. Steroid phobia is not a new phenomenon, however: a study in 1999 found that 72.5% of people expressed worry about using topical corticosteroids on their own or their child’s skin, with 24% admitting to not using their treatment as prescribed due to their concerns (Charman). Unfortunately, these numbers appear to be growing over time, at least in part due to the spread of information—and sometimes misinformation—facilitated by social media.
In reality, steroid phobia resulting in improper or under-usage of TCS is widely recognized by dermatologists as a frequent cause of failed therapy for eczema— thus making these fears a far more troubling problem, perhaps even more than the relatively small risk of developing significant side effects (Aubert-Wastiaux). It is therefore in the interest of both physicians and patients to demystify some of the myths surrounding TCS use and shed some light on a few misconceptions.
Guidelines for Using Topical Corticosteroids
According to the National Eczema Association (NEA) “Topical corticosteroids are recommended when patients have failed to respond to a consistent eczema skin care regimen, including the regular use of moisturizers (emollients), appropriate anti-bacterial measures, and trying to eliminate any possible allergens that may be contributing to the underlying problem.”
The NEA states TCS can be “applied once or twice daily for up to 14 days. Once or twice daily application is recommended for most preparations. More frequent administration does not provide better results. Low-potency steroids should be used on the face and with caution around the eyes.”
This a great systematic review of TSW from NEA in 2015 about how it is most likely caused from misuse of the medication.
When to Be Concerned
Dr. Peter Lio says “If things are getting worse or if you find you are using a topical steroid more than 2 weeks out of a month, then it is time to check in and/or get another opinion with another physician. Our basic goal is to be tapering off steroids, using less and less… with occasional flares perhaps. But if it is going the wrong direction, we need to hit the brakes!”
Myths vs. Reality Surrounding Topical Steroid Withdrawal
| Myth | Reality |
| Topical corticosteroids should not be used for the treatment of eczema due to the risk of local and systemic side effects. | TCS have been proven to be a safe treatment even in children when used carefully, and continue to be one of our most important therapies for calming inflamed skin and giving some relief to the suffering of eczema (Hajar). The incidence of reported side effects such as skin atrophy and growth retardation is very low, and is typically seen when very high potency TCS are used on thinner skin over long periods (see TCS usage guidelines above). Most side effects will resolve after discontinuing TCS use (Eichenfield). |
| Topical steroid withdrawal (TSW) is a worse version of normal TCS side effects.
| TSW is a unique adverse event that is separate from other topical corticosteroids side effects. It typically affects the face, neck, and genital areas, and is characterized by burning and stinging, worsening with heat or sun, itching, pain, and facial hot flashes upon stopping TCS therapy (Hajar). |
| Regular use of topical corticosteroids will result in TSW.
| A recent study reviewed 34 other studies from 1969 to 2013 and found that TSW results from frequent, inappropriate, and prolonged use of moderate- to high potency TCS (beyond the recommended TCS usage guidelines above) primarily on the face and genital areas. Appropriate use of TCS as prescribed is unlikely to predispose patients to TSW (Hajar). |
| All topical corticosteroids predispose patients to developing TSW equally. | Dermatologists prescribe an enormous variety of topical corticosteroids of varying strengths. Use of milder TCS like hydrocortisone is highly unlikely to predispose to TSW. The more potent the steroid, the shorter the duration of usage which can result in TSW (Ghosh). |
| TSW can be prevented by applying TCS less than prescribed, or “on and off” as needed, or only when symptoms get worse. | Not using TCS as prescribed may result in treatment failure, which may then require an even longer course and greater amounts of a potentially stronger steroid—thus actually increasing the risk of TSW. In this sense, proper short-term TCS usage may reduce the total amount of TCS needed to suppress inflammation in the long run, and thus minimizes the risk of acquiring TSW or corticosteroids side effects (Hon). |
| Once afflicted with TSW, the condition is irreversible. | TSW can be treated by discontinuing the TCS and providing supportive care, with or without the use of other non-steroidal treatments to help calm rebound symptoms. Phototherapy and cooling wet wraps may be used to help. While there is much yet to learn about TSW, it seems that nearly all cases will eventually improve. Importantly, many patients continue to have severe underlying eczema which can be confusing: this often will not improve over time, leading to some continuing to wait without treatment and suffering for months or even years without relief (Hajar). |
| Physicians can accurately predict the frequency/duration of TCS usage needed to prevent TSW. | Although TCS can be safely prescribed to avoid predisposing patients to TSW, there is still much that remains unknown about the condition. The exact rate of how common TSW is, as well as the minimum frequency and duration of TCS usage that can lead to it are still a mystery, making close follow up and frequent re-evaluation important for all eczema patients (Hajar, Ghosh). |
| Physicians can accurately predict which individuals may be predisposed to developing TSW. | The exact cause and process by which TSW develops is not fully understood, and it is currently unknown if there are other genetic or environmental factors that predispose individuals to developing it. For now, it appears that the single greatest predisposing factor is chronic misuse of TCS—especially those of mid- to higher potency— beyond the regimen that was originally prescribed (Ghohn). |
| Physical symptoms of TSW are easy to diagnose and are uniform among all patients.
| Physicians have yet to pinpoint the set of symptoms that are definitively associated with TSW, and there is variability in how different patients present. Some TSW symptoms also overlap with other conditions such as allergic contact dermatitis, further complicating the diagnosis. However, patients who experience any of the most common symptoms of burning/stinging, worsening with heat or sun, itching, and facial hot flashes within three weeks of stopping TCS usage should consult their dermatologist (Hajar). |
Related Posts:
Is It Just Eczema or Topical Steroid-Induced Eczema?
Common Allergens Found in Topical Cortisone – Could They Make Your Eczema Worse?
One Mom’s Journey To Hell And Back
Bio: Dr. Peter Lio is a Clinical Assistant Professor in the Department of Dermatology and Pediatrics at Northwestern University, Feinberg School of Medicine. He is the co-founder and co-directo r of the Chicago Integrative Eczema Center and very passionate about finding safe treatments that work for eczema. Dr. Lio received his medical degree from Harvard Medical School, completed his internship at Boston Children’s Hospital and his dermatology training at Harvard. He has had formal training in acupuncture under Kiiko Matsumoto and David Euler, and has held a long interest in alternative medicines. He currently serves on the Scientific Advisory Board for the National Eczema Association. His clinical office is located at Medical Dermatology Associates of Chicago.
r of the Chicago Integrative Eczema Center and very passionate about finding safe treatments that work for eczema. Dr. Lio received his medical degree from Harvard Medical School, completed his internship at Boston Children’s Hospital and his dermatology training at Harvard. He has had formal training in acupuncture under Kiiko Matsumoto and David Euler, and has held a long interest in alternative medicines. He currently serves on the Scientific Advisory Board for the National Eczema Association. His clinical office is located at Medical Dermatology Associates of Chicago.
References:
Aubert-Wastiaux, H., Moret, L., Le Rhun, A., Fontenoy, A. M., Nguyen, J. M., Leux, C., . . . Barbarot, S. (2011). Topical corticosteroid phobia in atopic dermatitis: a study of its nature, origins and frequency. Br J Dermatol, 165(4), 808-814. doi: 10.1111/j.1365-2133.2011.10449.x
Callen, J., Chamlin, S., Eichenfield, L. F., Ellis, C., Girardi, M., Goldfarb, M., . . . Wintroub, B. U. (2007). A systematic review of the safety of topical therapies for atopic dermatitis. Br J Dermatol, 156(2), 203-221. doi: 10.1111/j.1365-2133.2006.07538.x
Charman, C. R., Morris, A. D., & Williams, H. C. (2000). Topical corticosteroid phobia in patients with atopic eczema. Br J Dermatol, 142(5), 931-936.
Eichenfield, L. F., Tom, W. L., Berger, T. G., Krol, A., Paller, A. S., Schwarzenberger, K., . . . Sidbury, R. (2014). Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol, 71(1), 116-132. doi: 10.1016/j.jaad.2014.03.023
Ghosh, A., Sengupta, S., Coondoo, A., & Jana, A. K. (2014). Topical corticosteroid addiction and phobia. Indian J Dermatol, 59(5), 465-468. doi: 10.4103/0019-5154.139876
Hajar, T., Leshem, Y. A., Hanifin, J. M., Nedorost, S. T., Lio, P. A., Paller, A. S., . . . Simpson, E. L. (2015). A systematic review of topical corticosteroid withdrawal (“steroid addiction”) in patients with atopic dermatitis and other dermatoses. J Am Acad Dermatol, 72(3), 541-549 e542. doi: 10.1016/j.jaad.2014.11.024
Hon, K. L., Kam, W. Y., Leung, T. F., Lam, M. C., Wong, K. Y., Lee, K. C., . . . Ng, P. C. (2006). Steroid fears in children with eczema. Acta Paediatr, 95(11), 1451-1455. doi: 10.1080/08035250600612298

This is a very good article. I think TSW is real but thankfully is not too common. Still, people have to know about it as a risk!!!
My daughter went to dr. Lio. We lived him. He really helped aND listened. Her skin is way better!
That’s so wonderful to hear! We love Dr. Lio too!
thanks for this article.
i’ve taken my 3-year-old son to see several highly regarded dermatologists in the southern california area, and my family’s experience has been that they are too quick to promote the efficacy and safety of TCS, even long term, without looking at individual responses to the medication. we’ve had one “top doctor” tell us that TSA does not exist, and the reactions he saw on my son were an indication that my son needed more steroids, not less.
my hope is that dermatologists who patients and caregivers rely on during somewhat desperate times of eczema flare-ups will provide a more balanced view of safe TCS use as well as the possibility of TSA. i understand that many doctors in promoting the safety of TCS may be trying to counter the general fear that patients have at using TCS. but without closely monitoring patients for possible side effects and educating patients about them, they do a true disservice to the patient community.
several of my friends have received the same blanket advice from their dermatologists — that medium strength TCS are completely safe for long-term use. however, when we’ve explained to our doctors that our children have developed extreme redness and sensitivity on their faces where they’ve never had eczema before, or that they have not grown in height at their 6/12-month check-ups, nobody stops to question the possibility that there is a connection to TCS use. i’m not saying that TCS are to blame 100%, but why not act like scientists and problem-solvers and investigate further instead of blindly promoting TCS safety?
I think it is more common than they realize. But I am so very grateful that the dermatologists are finally recognizing it. It’s about time!!!
Thank you for posting about this. We need to get the word out! Many do not understand that this is real and brush it off completely!
My son went through TSW for 27 months. We started it the week after he turned 3 years old. He was prescribed topical steroids and oral steroids for 3 years. Peds and derms gave him steroids each time he was seen. One even gave him a steroid foam that was only for use in kids over age 12. He was 2. Just one more showing that dr’s don’t pay attention to the usage that is on the medication. When I brought it to her attention, she said oh it won’t hurt him just use it sparingly. TSW was the BEST thing we could have done. Yes, the 27 months was hell. He was pitiful looking. Swollen, weepy, cold, sleepy and miserable. Would I suggest others do that? Yes. Today, he is off of several medications and has not had one breakout of eczema since healing in 12/2014. Perfect skin.
So true. Somany peds do not even KNOWS about it! we have to TEACH they doctors to UNDERSTAND. This is a very good start because as you acknowledge the thing you can KNOW the thing! Right? ! Thanks you!!
1 thumb up/1 thumb down
This statement was inaccurate:
For now, it appears that the single greatest predisposing factor is chronic misuse of TCS—especially those of mid- to higher potency— beyond the regimen that was originally prescribed (Ghohn).
“Beyond the regimen that was originally prescribed”. I was prescribed TCS by my physician to use daily for YEARS in increasing doses and eventually given injections and prednisone. The physician was negligent and over prescribed the usage. I just followed his direction. I imagine many have experienced the same thing.
This statement was also inaccurate:
However, patients who experience any of the most common symptoms of burning/stinging, worsening with heat or sun, itching, and facial hot flashes within three weeks of stopping TCS usage should consult their dermatologist (Hajar).
“Within 3 weeks”… I personally sat in the waiting room of Dr. Rapaport’s office for my appointment and met a young girl having her 1st withdrawal/rebound from TCS cessation of 6 months. She was purple itching weeping swollen from head to abdomen. Her mom said she was totally fine for 6 months and then bam withdrawal. They were horrified. And I personally didn’t have my 1st flare til week 5/6. So the amount of time before withdrawal/flare can vary.
Overall the article was well written but a little off. I’m 51 months off steroids and still have withdrawals. They are different than eczema outbreaks. And each year the symptoms become less. I think there just isn’t enough data because there haven’t been enough studies and the medical community isn’t consistent with their treatment recommendations. Some doctors educate their patients and some don’t.
1 thumb up/1 thumb down
Seconding this. The reason I had to go through TSW twice (!!!) is because my dermatologist and multiple GPs kept precribing me steroid after steroid after steroid.
I was never once told anything about proper usage or potential issues. I was told during my first bout with TSW that it was just a mysterious eczema flare up that lasted over a year and left me nearly incapacitated. I was re-prescribed steroids just as I was beginning to get better. The second time it happened, I took matters into my own hand, did my research, and rode out withdrawal, and I emphasize this, AGAINST THE RECOMMENDATIONS OF MY DERMATOLOGIST.
That’s right. My dermatologist wanted me on steroids daily for the rest of my life. When I asked what the endpoint was (the weaker steroids had stopped working and I had been bumped up a strength level again when I began doing my own research), he basically shrugged and said hospitalization.
Too many doctors don’t do their research, don’t know the side effects of the medications they’re prescribing, and yet the patients are the ones vilified for ‘using medications wrong’. Compounding this, many doctors, confronted with a patient who has done research for themselves, refuse to even consider new evidence. It’s arrogant and it’s harmful and it completely ruined a decade of my life.
To the original writer of this article, please at least acknowledge that it’s often the doctors who are engendering misuse, not the patients. The only mistake I made was trusting my physicians implicitly.
It is impossible to say how “common” or “uncommon” the symptoms of topical steroid addiction are.
There are NO official figures on the incidence of TSA worldwide- this is because many doctors do not recognise it or because the symptoms present very similarly to eczema symptoms (rashes, itching burning etc). Therefore we do not know what percentage of TS users become addicted to the creams. In theory, millions of people could be dependent on steroid cream without realising it.
As someone who has been through TSA myself, I think that even a single sufferer is one person too many. I also know people who have used TS and had zero issues. Am I the exception or are they? Nobody knows. We need more information. That said, even if as few as 1% of topical steroid users became addicted, this could still translate to hundreds of thousands of people worldwide.
As TSA becomes better known, maybe we will get to the point where more data is available and we will have access to official numbers and percentages of those affected.
Until that time, it is presumptuous of anyone: doctor or layperson, to make statements of how widespread or rare the problem is without any official data and figures to back it up.
I don’t think corticosteroids is a solution, ever. It only delays the process of solving the underlying problem. And when eczema starts to spread, it is just dangerous to apply corticosteroids on such large skin area.
There are many people who have used topical steroid creams as prescribed and wound up suffering TSW when discontinuing the cream. I would recommend joining any number of the TSW support groups on FB to learn straight from the victims themselves. They are the experts in this area.
I love it when people who haven’t experiences TSW try and speak with authority on the subject. Until you’ve lived it, you don’t have a clue what you’re talking about (sorry) or what it’s about. The “inappropriate use” claim is infuriating. We used very little TS for a short period – every application per our Doctor’s instructions – and my son still suffered for 2.5 years to heal. The first year was a like horror film. There are no studies on it, no real data collection, so attempting to be an “expert” on this subject by looking at scientific papers is a joke. Your arrogance on this matter is shameful. Let the patients speak on this subject before you cause serious pain and illness in other children.
Hi Katie –
I’m sorry you feel this way. My son luckily did not suffer from TSW, to which I will forever be grateful. From what I’ve seen it’s very painful and emotionally draining in every possibly way. We’ve had a few different guest posts about TSW, so we wanted to share them on the blog to give multiple perspectives on the condition from a physician’s point of view and from someone who managed it personally and one from a parent whose child suffered from TSW. We hope that these posts can help shed some insight into this condition that has not been thoroughly researched. Thank you. Jennifer
I have a lot of respect for Dr. Peter Lio — at least he is trying to learn about and raising awareness about TSW — but this article is wrong on a couple fronts, already pointed out in other comments. This article puts the blame on patients for misuse of topical steroids, but the reality is that many doctors (the majority it seems) either don’t know about or don’t believe TSW is real, and they ignore the risks of steroids noted in the drug inserts. Many patients end up with TSW after relying on their doctors’ guidance. We did.
I think TSW is so-called “FAKE NEWS”. I think peopel from Eucrissa and Duplibumat company are trying to scare people off of using SIMPLE GOOD OLD FASHIONEDD STEROIDS!
STEROIDS ARE SAFE AND NATURAL. YoUR own body makes them. How can something NATURAL be unsafe?!
I think the drug company HATES how cheap steroids are and how effective–nobody makes enough MONEY MONEY MONEY $$$$$!!!
So they invent TSaW to scare people.
Wake up, sheeple. We’ve seen this before. Look at where the money goes.
-James Montgomery Flannigan, a concerned citizen who found out how much EUCRISSA and dimplimabs costed!
Asbestos is natural.
Arsenic is natural.
Anthrax is natural.
Natural does not mean safe. Just because our own body makes them, doesn’t mean they are safe (doesn’t mean they are dangerous either, but context, dosage, type of substance all play a role in the definition of ‘safe’).
Steroids made in a lab is not the same as steroids made in our bodies. Nor is the dosage we squeeze out of a tube the same as the dosage our bodies produce in the skin.
Blanket statements like the above are unuseful at best, harmful at worst.
Neither is calling suffering people, sheeple.